2023 Agenda
Understanding the Trifecta of Dental Distress: Anxiety vs. Phobia vs. Fear
Finnish researchers claim that one out of every two adults has mild anxiety of the dentist, while one in 10 is extremely afraid. What are the differences between these psychological emotions, and how best to help patients overcome them?
Let’s face it, dentists aren’t always faced with enthusiastic and elated patients. For those uneasy patients, their level of dread can vary – rooted in past traumatic experiences, all the way to a generalized fear of the unknown. Similarly, fear of doctors – also known as “white coat syndrome” – can be blamed for elevated blood pressure in those who normally have healthy levels.
While dental phobia is considered the most extreme, all three emotions (anxiety, fear, and phobia) can lead a person to completely avoid the dentist for decades, even a lifetime. Sedation dentists who understand these differences can help patients (and potential patients) overcome these psychological barriers, become regular patients, and realize a better quality of life through dread-free oral health visits.
Finnish Researchers Take an Innovative Approach

According to researchers at the University of Oulu, Finland (1), fear of the dentist is highly prevalent. While most people can manage to go to the dentist, some are reluctant and experience varying levels of anxiety and fear. But for a limited few, their powerful fear of the dentist is considered odontophobia. This is defined as a terror so intense that there’s a complete avoidance of the dentists until either the physical pain or emotional distress becomes too overwhelming.
Making global headlines for their innovative, multifaceted approach to this issue, the Clinic for Fearful Dental Patients (CFDP) in the City of Oulu, Finland aims to put a stop to dental anxiety, fears, and even the most extreme phobias.
This study followed patients treated at the CFDP. At the clinic, patients received care in a multifaceted approach. Patients at CFDP are treated by three dentists "who are interested in treating fearful patients and have taken courses on the topic," explains study author Vuokko Anttonen. Two are clinical practitioners who lecture at the University of Oulu on the topic of dental fear, and the third is a hypnotist.
From this, the long-term effects of the fear treatment period were studied. For example, whether or not patients visited their own dental clinics after their treatment at CFDP ended, if they stopped dental care altogether, and if/how often they required emergency dental treatment. This ten-year follow-up included a total of 152 patients from 2006-2016.
What Can Be Learned?
Younger patients, (2-10 years in age) had significantly more follow-up dental examinations than those treated over the age of 10. Preliminary success was associated with the number of examinations, but not with emergency visits and missed appointments. A link between fewer dental examinations and dental emergency care needs was associated with unsuccessful dental fear treatment.
From this, researchers concluded that dental fear treatment at an early age is the most beneficial, and successful treatment has a positive impact on dental care and regular dental attendance. Meaning, without successfully treating the psychological factors, the initial positive results diminish over time. For those patients, dental distress is something that must be addressed throughout their lifetimes, perhaps with a focus on the multifaceted approach the CFDP took – treating both the oral health and psyche of patients.
Not All Emotional Distress Is Equal
Unfortunately, the terms dental fear, dental phobia, and dental anxiety are often seen as interchangeable – but they aren’t. Here's how to distinguish the differences.
- Dental Anxiety: This is seen as a fear of the unknown and comes from a generalized anxiety around dentists. According to Dental Fear Central, most people have some degree of dental anxiety, especially for more involved procedures that are new to the patient. However, dental anxiety isn’t necessarily responsible for complete avoidance.
- Dental Fear: Dental fear is specific and often arises from a past traumatic experience. If a patient can tell you exactly what they’re scared of (gagging, suction, drills, or needles) this is considered dental fear. It’s also common to have more than one dental fear, and these fears can keep patients from regularly visiting the dentist.
- Dental Phobia: The most intense of dental distress, dental phobia can be so powerful that those suffering from it can avoid the dentist indefinitely, only to seek emergency care when the physical pain becomes too overwhelming. Some people with dental phobia might still visit a dentist but do so with intense dread.
Treating The Whole Patient
It’s important for dentists to remember there's a wide variety of techniques and tools available to treat dental fear disorders including, but not limited to sedation.
Dental Fear Central is a great resource for dentists, students, and allied professionals seeking to treat the trifecta of dental fear. They provide patient insight, stories, tips, and resources. While it’s a United Kingdom-based website, they offer technology, courses, and highly relevant resources useful for dental professionals everywhere.
Here are a few recommendations that apply to patient anxiety, fear, and phobias. The level and exact method for each person is unique to their situation.

- Relinquish control. For some patients, their fears center around the loss of control. Remember that patients will look for a dentist that fits their needs. Have a conversation with the patient to discuss their unique situation and give them the power to signal that they need a break from the treatment. Agree to a sign such as a hand raise during treatment, so you’ll know when to stop, giving the patient some comfort in control.
- Show empathy/understanding. Be genuine and sincere when communicating with patients. Don’t pass judgment or chastise them for a lack of dental care. Instead seek to understand and listen.
- Take it slow. Let the patient know their first checkup won’t involve complicated or painful procedures. After that, make appointments at their pace. Some might benefit from longer appointments, others from shorter and more frequent ones.
- Be on time. Tick tock. Tick tock. The worst way to start an appointment with an anxious patient is by making them sit in the waiting room or in the operatory alone with all the dental equipment contemplating the worst-case scenario.
- Distractions are up to the patient. Many dental practices are now using televisions, iPads, or music to distract patients. However, for some, this can actually act as an instigator to their anxieties and fears. Let them decide what type of media, as well as the sound level used to distract them.
- See the experience through your patients’ eyes. Sit in the waiting room, walk back to the operatory and pay attention to the details. Is there clutter? Loud talk about patients in front of other patients? How’s the aesthetics of your office? When is the last time you walked in their shoes?
In Conclusion
It’s important to realize that working with fearful patients can be difficult and requires more time and effort on the dental professional’s part. For many dentists, caring for others is one of the driving factors in choosing their profession and facing these challenges can be rewarded tenfold. When doctors help patients overcome their fears, anxieties, or phobias they’ll often discover a truly devoted patient who’s likely to spread the good news to others.
References:
1. Kankaala, T., Laine, H., Laitala, ML. et al. 10-year follow-up study on attendance pattern after dental treatment in primary oral health care clinic for fearful patients. BMC Oral Health 21, 522 (2021). https://doi.org/10.1186/s12903-021-01869-6
Safe Sedation: Understanding Your Patient’s Recreational Drug Use
Sedation safety requires knowing your patients' complete health history. However, depending on your state, your patients might hesitate to disclose their use of recreational drugs.
After California legalized medical marijuana (aka cannabis) in 1996, 39 states and the District of Columbia have since legalized it for medical use, while 21 states and the District of Columbia have legalized cannabis for recreational use.
Following in the footsteps of cannabis, there's a growing movement (from both sides of the political aisle) to decriminalize and legalize psychedelic drugs known as psilocybin (magic mushrooms) or LSD. In fact, Oregon (in 2020) and Colorado (in 2022) legalized psilocybin and micro-dosing LSD under certain conditions.
Since the 1960s and 1970s, certain recreational drugs have experienced a psychedelic renaissance. Back then, psychedelics carried a negative stigma that kept them out of mainstream healthcare – and conversations. However, thanks to technological advancements in medicine and the increased popularity of having health benefits, their negative stigma has dissipated, as has the suppression of discussing them. As attitudes toward these drugs continue to evolve, patients are more likely to share with you that they're using them.
Alcohol
Alcohol contains ethanol, produced through fermentation of sugar-containing sources, of 3-50%. Thirty-three percent of people worldwide consume alcohol, and 86 % of Americans have consumed it in their lifetime.
Knowing a patient's alcohol intake before a procedure can give you helpful clues, such as how much they'll bleed during the surgery. Alcohol also acts as a competitive inhibitor of other medications, making other drugs more potent.
Pharmacodynamic: Alcohol enhances the effects of the medication, particularly in the CNS (for example, sedation medications). Combining alcohol with other CNS depressants increases the risk of overdosing.
Many medications interact with alcohol, including antibiotics, antidepressants, barbiturates, benzodiazepines, Warfarin, anticonvulsants, and more.
Sedation candidates should not consume alcohol the day before and the day of the sedation appointment. Alcoholics who are physically dependent and not in a successful recovery are not acceptable candidates for sedation in the outpatient setting.
Cannabis (Marijuana)
Federally illegal but legal state-by-state in the U.S., it's crucial for dentists to realize that cannabis use (either recreational or medical) is highly common. It's also no longer something dentists should assume patients will volunteer to tell you. Instead, medical professionals should be forthcoming in asking the question. Given its commonality, patients feel more comfortable discussing cannabis use with their doctors.
Tetrahydrocannabinol (THC), the psychoactive component of cannabis, causes euphoria, an altered sense of time, difficulty concentrating, and impaired short-term memory and coordination. Its impact on sedation is relaxation, antiemetic, and increased heart rate.
When combined with sedative medications, some science suggests cannabis will make nausea worse, while others suggest it will lessen it. However, nausea and vomiting in sedation patients can be dangerous, so precautions are advised. Additionally, despite being a CNS depressant, cannabis can cause tachycardia, discomfort, and a potentially hazardous situation in sedation patients.
Cannabis Use and Sedation Patients:

- Dentists should ask patients how long they've used cannabis. How often? How much? And in what form?
- Evaluate for respiratory disease.
- If they are a heavy user or long term, ask about nausea and vomiting and consider using antiemetic prophylactically.
- Patients must withhold use on the day of sedation.
- Whenever possible, keep sedation appointments to three hours or less.
- Monitor HR closely when using vasoconstrictors.
Cannabis Drug Interactions
- CNS depressants may enhance the CNS depressants of cannabinoids.
- CYP3A4 Inhibitors (e.g., Clarithromycin, Diflucan) may increase the serum concentration of THC.
- Vasoconstrictors may enhance the tachycardia effect of cannabis.
- All interactions are [C] level interactions according to Lexi-Comp.
Cannabidiol (CBD)
- Not psychoactive compared to THC.
- May reserve THC intoxication or sedation.
- Inconclusive data to support its use in the treatment of anxiety or pain.
- Epidiolex was approved in 2018 by the FDA for the treatment of two epilepsy disorders
- Same drug interactions as THC.
- Same treatment recommendations with sedation as with THC.
Patients should not use recreational CBD and cannabis on the day of the sedation appointment. However, medically approved cannabis and CBD should be treated like every other medically prescribed drug and should be taken on the day of the appointment.
The FDA has not approved the cannabis plant for medical purposes. However, individual cannabinoids have been approved by the FDA for use in medications.
Epidiolex contains a purified form of CBD derived from cannabis and has been approved for treating seizures associated with severe and rare forms of epilepsy called Lennox-Gastaut syndrome and Dravet syndrome.
The FDA has also approved Marinol and Syndros, which contain dronabinol (synthetic THC), and Cesamet, which contains nabilone (a synthetic substance similar to THC). In addition to treating nausea and vomiting caused by chemotherapy, dronabinol is also used to treat loss of appetite and weight loss in HIV/AIDS patients.
Lysergic Acid Diethylamide (LSD)
- AKA "Acid".
- Potent psychedelics are used primarily as recreational drugs.
- Causes mental, visual, and auditory hallucinations.
- Long duration of action of up to 20 hours.
- The mechanism of action is not precise, although agonism of serotonin and dopamine receptors is suspected.
- A low dose to increase creativity and productivity is called micro-dosing.
- Considered to have low addiction potential for use.
- LSD is designated as a Schedule 1 drug. (Federally illegal for medical and recreational use)
Side Effects Include:
- Cardiovascular stimulation.
- Respiratory impairment.
- Nausea and vomiting.
- Tremors.
- Psychological aberrations.
LSD Use and Sedation Patients:
- CNS depressants tend to dull the effects of LSD.
- Benzodiazepines treat LSD overdose as they decrease central and peripheral sympathomimetic drug effects.
- Mixing lithium, TCAs, or CNS stimulants with LDS can be lethal.
- Providing sedation to any patient under the influence of a psychedelic drug is contraindicated. The pattern of LSD used must be determined. The half-life of LSK is 3.6 hours. At 14.4 hours, 90% of the drug is expected to have been eliminated.
Dentists should ask about this drug use, specifically if practicing in Colorado, Oregon, or California. If the patient answers yes, have them withhold use the day before and the day of the appointment. Monitor vasoconstrictors carefully and proceed judicially.
Psilocybin (Magic Mushrooms)
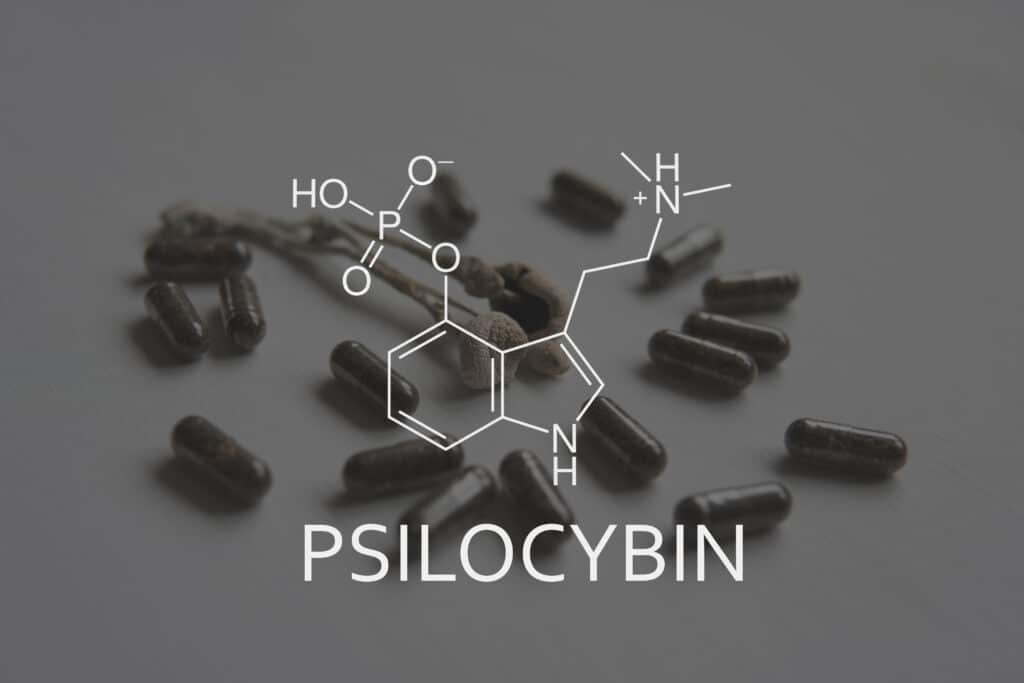
Psilocybins, aka "magic mushrooms," are substances obtained from certain types of naturally occurring mushrooms. These mushrooms are consumed by ingesting fresh or dried fruit bodies that cause hallucinogenic effects. Activity occurs once it is metabolized into psilocin, which acts on serotonin receptors in the brain. Magic Mushrooms have a duration of action of 2-6 hours and do not cause physical dependence.
Effects:
- Pupil dilation.
- Panic attacks.
- Nausea.
- Hypertension.
- Tachycardia.
- LD50 is 280 mg/kg or 150% of the LK50 for caffeine.
Psilocybin Use and Sedation Patients:
- Patients should refrain from using it on the day of sedation.
- As a precaution, use vasoconstrictors judiciously and monitor closely.
- Due to additive CNS depression, administer sedation medications low and slow.
Have That Conversation
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), more than 59.3 million people (ages 12 or older) used "illicit" drugs in 2021. While opinions can vary on recreational drugs, sedation requires the provider to know all the drugs (legal or otherwise) your patients are taking.
Identifying recreational drug use can be a delicate matter for some patients. Therefore, healthcare practitioners should also realize that some patients may be reluctant to share such information for fear of judgment.
Yes – sedation dentists need to be aware of their patients' full drug history, but not by being so forward that they become fearful or hesitant to share such an essential part of their medical history. The most straightforward approach is including a question about recreational drug use in the medical history questionnaire and reassuring the patient that these are entirely confidential and only used as a preliminary scan for their health.
Another aspect to consider is how recreational drugs interact with other medications, mainly analgesics and sedatives. Dentists must be aware of the patient's drug use so their heart rate can be more closely monitored when using vasoconstrictors.
Test Your Knowledge: Home Care Instruction for Sedation Patients

Providing follow-up care to sedation patients requires planning and specific communication strategies. For the 15th Annual Safe Sedation Week, we review the recommendations for thorough oral hygiene and home care instructions.
When hygiene services are provided to sedation patients, the typical oral hygiene instructions (OHI) and home care instruction (HCI) process differs from traditional procedures. Because the patient is sedated during their treatment, it’s recommended they complete their OHI during 3-4 separate visits, each about 15-20 minutes long.
Basic Oral Hygiene Instruction Prior to Treatment
Initial HCI should always be provided prior to the planned sedation procedure so that patients can take appropriate measures to prepare. In most cases, instructions can be incorporated into the exam or consultation appointment after a patient accepts a recommended treatment plan. These 10-15 minutes of OHI serve both for educational purposes as well as establishing a personal rapport with the patient. It also creates the opportunity for personal investment from the patient in regard to the success of their treatment.
During the initial home care session, keep instructions basic. Brushing and flossing are all that you need to cover at this pre-treatment meeting. It’s not yet necessary to overwhelm the patient with more specialized types of oral hygiene devices.
On the Date of the Procedure
On the date of the procedure, the focus should be specifically on the treatment being rendered. Since the patient will be sedated, it’s unlikely that they will accurately remember any HCI provided at that time. However, you may as a courtesy review basic HCI with their escort and provide a written copy of the OHI instructions provided at the previous appointment as a refresher. This step allows the escort to ensure the patient is being looked after properly and serves as a reminder to the patient as their sedatives wear off.
One Week Follow-Up

Have the patient return for a one-week post-op visit to assess their response to treatment. After a periodontal debridement or scaling and root planing have been completed, you’ll have a better idea of the patient’s specific oral hygiene needs. Including any specific tools, products, or techniques that should be utilized around localized areas of their mouth.
During this appointment, re-evaluate their oral hygiene methods and introduce new techniques or products that may have previously been more challenging to use. Such as floss threaders, proxy brushes, or subgingival irrigation devices. Use the opportunity to reassure the patient of the progress that’s already been made. Reaffirm how their investment in their prescribed HCI has amplified their response to their periodontal procedure. Now is the time to adjust things further, specifically in the hopes of avoiding disease relapse in at-risk areas of their mouth.
Because you are introducing new oral hygiene techniques and devices, be sure to also provide a written copy of OHI at this appointment.
One Month Follow-Up
From here, a third hygiene instruction visit should be scheduled either at the four-week mark or following the completion of prescribed restorative treatment. At this time, review the overall progress of the patient’s soft tissue healing and their oral hygiene efficacy. Reassure them of the progress they’ve made thus far. Go back and review any brushing, flossing, or adjunctive device use as it relates to specific areas of concern.
These recurring home care sessions need not last more than 15-20 minutes each.
Continuing Care
Placing the patient on a re-care or periodontal maintenance schedule at appropriate intervals will allow for gentle reminders of past OHI, providing the assurance the patient needs to play an active role in the improvement of their oral health. Encourage your patient to continue incorporating each aspect of their oral hygiene routine. Not just for the purpose of tooth preservation and systemic health, but also to reduce the extent of treatment needs in the future, including additional sedation procedures.
Altogether, these oral hygiene educational reviews educate, remind, and prompt patients in a manner that isn’t easily overlooked, even given the use of sedation.
Sedation Training for Hygienists
Implementing sedation in the dental practice allows hygienists to collaborate with dentists for comprehensive patient care and fewer appointments. Trained dental hygienists can safely provide the same level of care to their patients without eliminating the personal OHI or HCI process that frequently accompanies the typical recall appointment.
Providing safe sedation services during necessary hygiene procedures expands the accessibility of care for patients experiencing severe anxiety, dental phobia, or who otherwise delay treatments because of the complexity of their oral health needs. In turn, hygienists can provide their sedation patients with the reassurance that their periodontal treatment will play a long-term, positive role in the future of their smile.
Sedation Dentistry: Improving Access and Quality of Care for Special Needs Patients
Recently, the push to improve access to oral health care for patients with physical, developmental, and mental disabilities has increased. Through sedation dentistry, care can be tailored to meet the individual needs of these patients, ensuring a safe, comfortable, and stress-free dental experience.

In America, disabled patients needing to see the dentist often wait years for qualified care. While some are fortunate and find faster treatment through special programs at dental schools, many with severe developmental, physical, and mental disabilities can only undergo dental procedures under general anesthesia – which is costly and difficult to find.
Adding to the problem, special needs patients may experience increased oral health problems due to sensitivities, nutrition, difficulty brushing, and access to dental care. This can increase caries, gum disease, and other oral health problems.
Special needs patients also experience increased hurdles when seeking routine preventive care such as professional cleanings and exams due to the availability of properly trained dentists. Because of this, many people with special needs suffer from rotting teeth, inflamed gums, and chronic pain that severely impacts their health and quality of life.
Is Sedation Dentistry the Answer?
Sedation can be an effective tool in the dental management of patients with special needs. In addition, sedation can help decrease their dental anxiety and fear, allowing dentists to complete treatments more efficiently and effectively.
As such, the dentist must select specific sedative drugs that are safe and effective based on their unique needs. Sedation dentistry can also help to reduce the need for more invasive forms of treatment and can help to reduce the risk of physical and psychological trauma associated with dental care for special needs patients.
A Crisis of Care
In a St. Louis Post-Dispatch article by Michele Munz, Sallye Holland of St. Louis details the painful struggles that her daughter Cassandra Holland faces in finding the high level of dental care she needs.
In addition to being mute, Cassandra has epilepsy related to her spastic quadriplegia cerebral palsy, keeping her in a wheelchair. In the article, Sallye recalls her harrowing struggle to find dental care for Cassandra, often ending up in the emergency room where she was prescribed antibiotics and sent on her way, only to repeat the cycle all over again.
It was a year ago when Cassandra finally found hope. As one of the first patients to get care through a program created by Barnes-Jewish Hospital, the dentistry school at A.T. Still University (ATSU-MOSDOH), Washington University School of Medicine in St. Louis, MO, and Affinia Healthcare, Cassandra finally received the dental care she desperately needed. Sallye remarks how emotional she gets when retelling this story. Thanks to a kind person on the other end of the phone at Barnes-Jewish Hospital, "…It was everything. That's when things started changing for us."
Robert J. Schmidt, DDS, who prompted the clinical collaboration, stated on Washington University's website: "Half a million people in the St. Louis area are living with disabilities, but few dentist offices accept special-needs patients, and even fewer accept Medicaid."
Advocacy for Special Needs Oral Healthcare

The St. Louis area collaboration was part of a broader effort led by Affinia Healthcare and ATSU-MOSDOH to ensure equal access to "quality emergency and comprehensive dental care" for residents of St. Louis.
Founded in 2015, St. Louis Dental Center provides comprehensive, affordable oral health care to patients of all ages to address the lack of oral health services for underserved, vulnerable populations. Since 2017, the Center has treated 230 patients with special needs. Despite this, some patients' needs still exceed the Center's capabilities, and their waiting list has only grown.
Considered a significant win in 2022 for special needs patients, the Centers for Medicare and Medicaid Services (CMS) established new dental billing and payment arrangements to improve access to hospital-based operating rooms requiring general anesthesia for dental procedures. By revising this arrangement, dental providers can now provide complex dental treatments for these patients faster while receiving more timely and fair reimbursement.
In California, the 2022-23 state budget signed by Governor Gavin Newsom included all of the California Dental Association's (CDA) top requests. This includes investing in workforce development in healthcare, $50 million for new and expanded infrastructure to serve special needs dental patients, and $10 million to develop clinical rotations for dental students further.
In Conclusion
In 2022 we saw oral healthcare reform play out nationwide and give a greater voice to those with the most need. At the federal level, the Fiscal Year (F.Y.) 2023 omnibus appropriations bill includes an increase of 3.5% for oral health across the board, with dental research and Indian dental health as significant benefactors. This is a promising sign as modern healthcare seeks to meet the growing diversity of patients where they are, sometimes with the most unique needs and in the hardest-to-reach places.
With the inclusion of sedation dentistry, special needs patients can find appropriate treatment and gain an increased quality of life. By providing patient-centered care and techniques, sedation dentistry helps special needs patients access a more comfortable, stress-free dental visit that can improve their overall wellbeing.
2023 Safe Sedation Dentist of the Year: Rasheeda Johnson, DDS, MBA

This year's choice as Dentist of the Year for the 15th Annual Safe Sedation Week is on a literal and figurative mission. From starting at a young age as an unofficial dental assistant in a family friend's practice, to co-founding a worldwide non-profit, Rasheeda Johnson, DDS, MBA, has always been determined to be where she can make the most difference.
After receiving technical training in a high school program, Dr. Johnson majored in Health Science at Hofstra University and then pursued her dental education at Howard University College of Dentistry. She completed a one-year General Practice Residency at Nassau University Medical Center and earned an MBA with a Marketing Specialization from Louisiana State University Shreveport.
Dr. Johnson's desire to learn has expanded into orthodontics, implant surgery, BOTOX® for TMJ symptoms, and more. She was introduced to the DOCS Education programs early in her career, learning oral conscious sedation in 2015 and adding IV sedation in 2021. Dr. Johnson found that implementing sedation allowed her to close more cases of anxious patients and those who were difficult to treat otherwise.
Dental Helping Hands
While in dental school, Dr. Johnson and two fellow students took several mission trips to Africa to provide oral healthcare to underserved communities. With encouragement from a member of the embassy in Sudan, she launched Dental Helping Hands in 2016 with her classmates.
Since then, the non-profit group has been offering free dental care and education to rural villages in several countries, including Ghana, Jamaica, Tanzania, and Nigeria, as well as here at home in Virginia. In addition, two of the six board members are oral surgeons, allowing them to provide cleft lip and palate surgeries.
Access to a medical facility may be hours away for many villagers who can barely afford where they're living, much less own a car, so being able to bring care to them has been fulfilling, explained Dr. Johnson.
"Even though it's a small thing I'm doing – it might be an extraction or a filling … this person, they really need it." She added, "It's instant gratification because you know the people you're treating don't have access to care in the way you do."
"I Want to Go Where People Aren't Going."

Dr. Johnson's unique perspective on instant gratification has defined her career even between international missions. She provided dental care in several U.S. locations, including a clinic in Maryland for special needs children and adults. When Floyd Lee Locums, a healthcare staffing company, offered her more opportunity to travel domestically, she accepted. It wasn't until later that Dr. Johnson discovered she'd be providing much needed oral healthcare to prison facilities nationwide. Yet again, she enjoyed helping all of her patients with inadequate dental access, and they were grateful for her care.
"It was the most organized place I've ever worked," she laughed.
Eventually, this position showed her how much she could accomplish here at home, and Dr. Johnson's 'why' became entirely centered around helping the people who may not have easy access to care.
"I want to go where people aren't going, where people aren't being serviced," she said.
This lack of access included patients who needed care outside of the typical 9-5 schedule. In response to this issue, Dr. Johnson and Dominique Bonner, DDS, opened Dentcare Now in Fairfax, Virginia in 2019. In addition to urgent services, the practice also offers a wide spectrum of dental and surgical care, including:
- Pediatric
- Restorative
- Cosmetic
- Sedation
- Endodontics
- Orthodontics
- Digital technology
- One-visit crowns and restorations with CEREC®
The office also provides a "Comfort Menu" with items such as Wi-Fi, headphones, VR technology, stress balls, and spa offerings to further relax nervous patients.
Looking Ahead
One would think Rasheeda Johnson's plate would be full now, but she's always looking for other communities to help – including nursing homes and the senior population.
"I haven't really touched that yet," she said, adding that she hopes to add mobile services as an extension of the surgical center as well.
Additionally, her goal is to take four mission trips annually, incorporating personal travel with the non-profit's work.
Dr. Johnson is currently the only one at Dentcare Now who provides sedation. Still, she was recently inspired after a recertification program to further train her team in order to serve more patients. She also plans to take a Master Series program this year to help a broader range of medical cases and patient populations.
In her limited free time, Dr. Johnson enjoys being active, working out, traveling, and spending time with friends and family. However, she admitted a hope to achieve more balance in her life and slow down a little bit. When asked about her future plans, she replied with a laugh, "Take a nap!"
That sounds like well-deserved instant gratification.